Preparing for a Bone Marrow Transplant: What Patients Need to Know
Know This Before a Bone Marrow Transplant
A bone marrow transplant (BMT) is a critical medical intervention employed to save the lives of patients with specific cancers, blood disorders, and immune system deficiencies. While it provides hope for recovery, the process can be taxing both physically and emotionally. Preparation on all fronts, mental, physical, and logistical, can greatly enhance both the experience and the results.
Patients can consult this guide to gain a comprehensive understanding of essential information regarding bone marrow transplants, including how the procedure works and how to manage expectations during recovery.
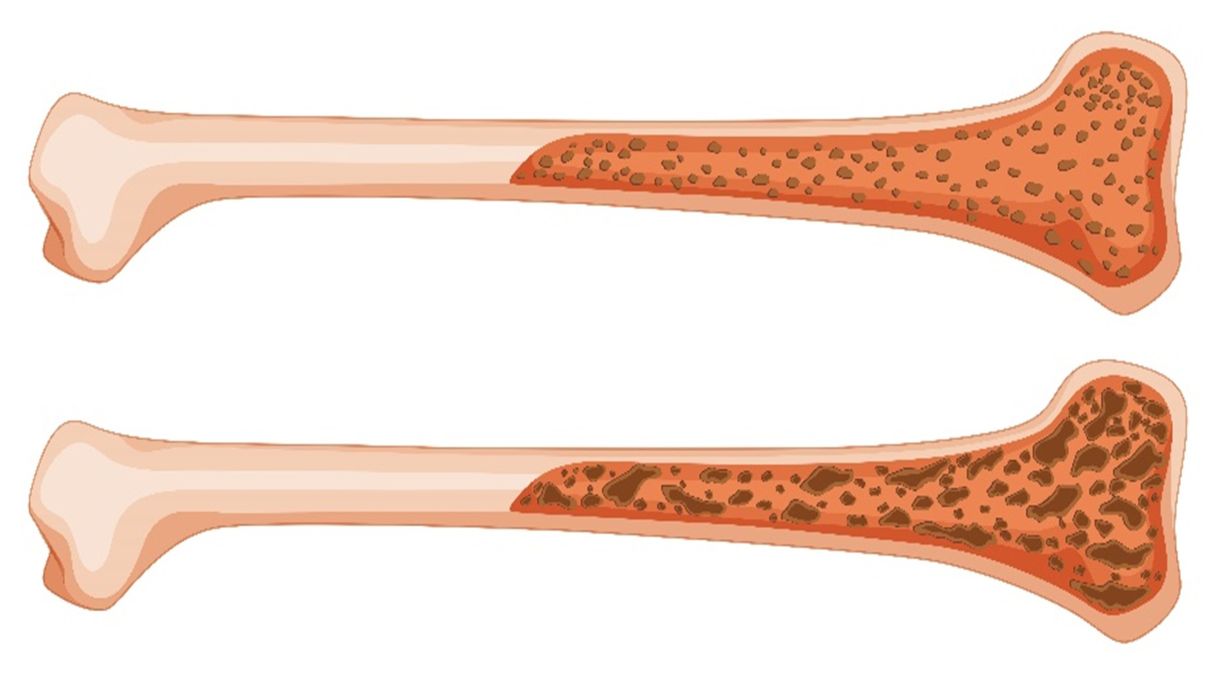
What Is Bone Marrow?
The soft, spongy tissue found within bones that generates blood cells—such as red blood cells, white blood cells, and platelets—is known as bone marrow. A transplant may be needed to restore healthy cell production when the marrow is diseased or damaged.
What Is a Bone Marrow Transplant?
A stem cell transplant, or bone marrow transplant, involves replacing damaged or destroyed bone marrow with healthy stem cells. These cells may originate from:
- Autologous transplant: utilizing stem cells from the patient
- Allogeneic transplant: utilizing donor-derived stem cells
- Haploidentical transplant: utilizing a half-matched donor, frequently a relative
- Umbilical cord blood transplant: utilizing stem cells derived from umbilical cord blood
The kind of transplant is determined by the patient’s diagnosis, health condition, and the availability of donors.
Who Needs a Bone Marrow Transplant?
Common conditions requiring BMT include:
- Leukemia (especially acute forms)
- Lymphoma (Hodgkin’s and non-Hodgkin’s)
- Multiple myeloma
- Aplastic anemia
- Sickle cell anemia
- Thalassemia
- Certain inherited metabolic disorders
When standard treatments such as chemotherapy or radiation are unsuccessful, a transplant is often the final option.
Pre-Transplant Evaluation and Preparation
- Medical Evaluation: Prior to the procedure, you will have comprehensive tests conducted to evaluate your physical readiness for the transplant. Tests could encompass:
- Blood and urine tests
- Imaging scans (X-rays, CT scans)
- Heart and lung function tests
- Dental and infectious disease screening
The aim is to identify and handle any underlying problems that may complicate recovery.
- Finding a Donor: When an allogeneic transplant is necessary, physicians will search for an appropriate HLA match (human leukocyte antigen) in:
- Family members, typically siblings
- Donor registries at the national or international level
If a complete match is not available, partial or haploidentical matches can be taken into account.
Pre-Transplant Conditioning (Preparative Regimen)
What Is Conditioning? Conditioning comprises the application of high-dose chemotherapy and/or radiation therapy prior to the transplant. This is intended to:
- Eliminate cancer cells
- Weaken the immune system to avert rejection
- Make room for new stem cells in the bone marrow
There are two types:
- Myeloablative conditioning: characterized by intensity and aggressiveness, frequently applied to patients who are younger or in better health
- Reduced-intensity conditioning (RIC): gentler approach, applied to older or more vulnerable patients
Side Effects to Expect:
- Fatigue
- Nausea and vomiting
- Hair loss
- Mouth sores
- Increased risk of infection
Depending on their response and recovery, patients are often advised to prepare for a hospital stay of 2 to 6 weeks.
Preparing Emotionally and Logistically
- Mental and Emotional Preparation: A transplant places a heavy emotional burden. It’s usual to feel:
- Anxiety or fear
- Sadness or depression
- Loneliness during isolation
Ways to prepare:
- Consult a psychologist or counselor.
- Become part of a support group
- Communicate openly with relatives and caregivers
- Organizing Aid and Logistics Designate a caregiver: There should be a person available around the clock during and following discharge
- Time off from work/school: You might require a few months for recovery
- Financial planning: Consult with your healthcare professionals regarding insurance coverage and expenses
- Ready your home: Guarantee tidiness and infection management
The Transplant Procedure
Day of Transplant – Often Called “Day 0”: Infusing stem cells is not complicated and is similar to a blood transfusion. Usually, it is not painful and lasts a few hours.
Post-transplant days are noted as Day +1, Day +2, etc., to track recovery milestones.
Post-Transplant Recovery: What to Expect
- Hospital Stay: Post-transplant, patients are observed for complications such as:
- Infections (resulting from low white blood cell counts)
- Graft-versus-host disease (GVHD) occurs in allogeneic transplants
- Organ Toxicity
To lower the risk of infection, you will stay in an isolation room and may require transfusions or antibiotics.
- Engraftment: Engraftment refers to the process by which the transplanted stem cells start to proliferate and generate healthy blood cells. This usually happens 10 to 28 days after the transplant. Your progress will be tracked through blood tests.
- Side Effects and Complications: Common issues include:
- Low appetite
- Rashes or skin problems
- Diarrhea
- Fever
Serious risks:
- GVHD (in allogeneic transplants): occurs when donor cells attack the patient’s tissues
- Organ damage: liver, lungs, or heart
- Relapse: return of original disease
- Close follow-up care is critical in detecting and managing these.
Life After Transplant
- Recovery of the Immune System: After the transplant, your immune system will stay weakened for 6 to 12 months. In this period:
- Stay away from places that are crowded
- Use masks in public places
- Only consume food that is well-cooked
- Avoid contact with ill people
- Continue vaccinations according to the doctor’s recommendation
- Long-Term Medications: You may be prescribed:
- Immunosuppressants (especially in allogeneic transplants)
- Antibacterials, antifungals, and antivirals
- Supplementation for nutrition and bone health
Nutrition and Lifestyle
- Emphasize a diet that is low in fat and rich in protein.
- Keep your hydration up
- Steer clear of foods that are raw or not fully cooked.
- Add in light exercise as endurance builds
Your care team may include a dietitian and a physiotherapist.
When to Call Your Doctor
Even after discharge, be vigilant about symptoms such as:
- Fever over 100.4°F (38°C)
- Chills or night sweats
- Unexplained bruising or bleeding
- Shortness of breath
- New rashes
- Diarrhea lasting more than a day
Timely medical intervention can prevent complications from worsening.
Related: Nutrition and Lifestyle After a Bone Marrow Transplant
Although a bone marrow transplant is a difficult process, proper preparation, support, and medical advice can result in restored health and vitality. It necessitates physical power, emotional toughness, and a robust support network. It is essential to understand the process, manage expectations, and communicate closely with your healthcare team.
For those who are getting ready for a bone marrow transplant—whether it’s you or someone close to you, expert treatment at L H Hiranandani Hospital is worth considering. The hospital provides world-class care tailored to each patient’s unique needs, with state-of-the-art transplant facilities, an experienced team of hematologists and transplant specialists, and comprehensive pre- and post-transplant support. The right team is essential for your recovery journey—rely on Hiranandani Hospital to lead you through each stage.
FAQs
1. How long does it take to recover after a bone marrow transplant?
The recovery period can differ from person to person, but the majority of patients start to notice improvements within 3 to 6 months post-transplant. Depending on the kind of transplant and personal health considerations, a complete recovery that includes immune system rebuilding can take up to a year or more.
2. What should I eat before and after a bone marrow transplant?
A diet high in protein and rich in nutrients helps get your body ready for treatment prior to the transplant. Once the transplant is complete, your medical team will suggest a neutropenic (low-bacteria) diet to mitigate the risk of infection. This typically involves consuming well-cooked foods and pasteurized products, as well as avoiding raw fruits and vegetables unless they have been peeled and washed.
3. Is it safe to be around family and friends after the transplant?
Yes, but carefully. Your immune system is weakened in the early recovery phase. Avoid contact with sick individuals, keep good hand hygiene, and limit your exposure to large crowds. As your immune system recuperates over time, you can slowly increase social interactions with your doctor's advice.